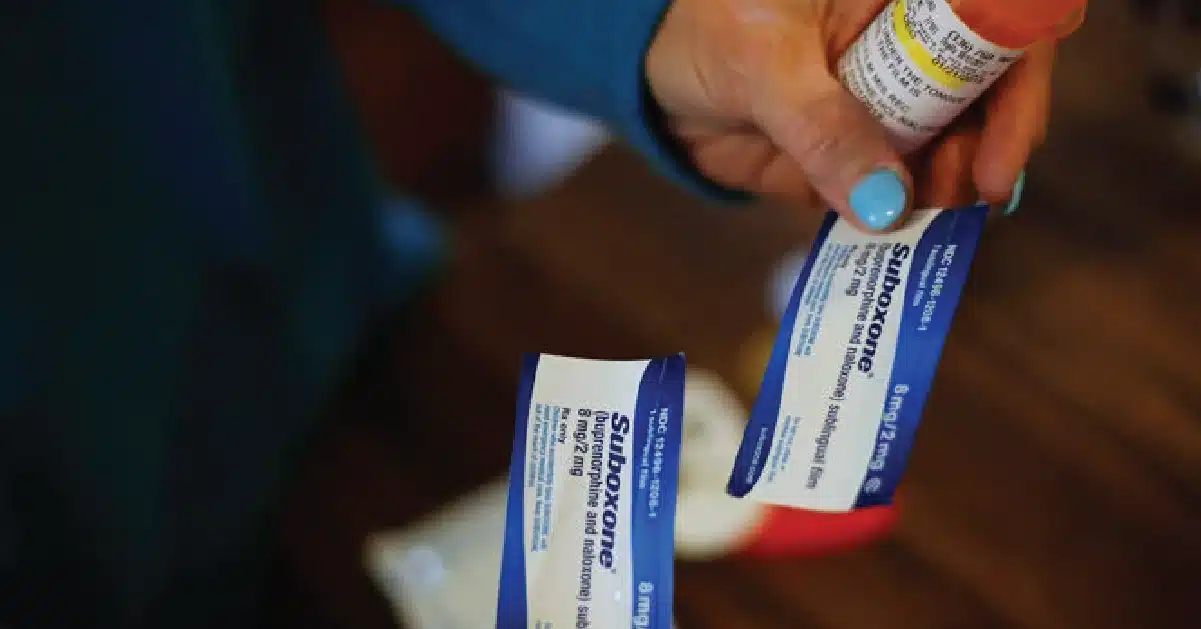
Suboxone is a combination of buprenorphine and naloxone used to mitigate opioid withdrawal symptoms and cravings.
As a revolutionary form of medication-assisted treatment, Suboxone helps individuals gradually overcome opioid dependence. While it proves effective in supporting recovery, concerns arise regarding its potential for abuse, especially among teenagers.
Understanding the delicate balance between its healing properties and the potential for misuse is crucial for fostering responsible usage in the fight against opioid addiction.
Key Takeaways
Regular medical supervision is crucial during Suboxone treatment to monitor progress, adjust dosage, and address any emerging concerns or side effects. Here’s what the article touches upon:
- Suboxone is an evidence-based medication for opioid use disorder, effectively reducing cravings and withdrawal symptoms.
- It works by binding to the same receptors in the brain as opioids but with a lower risk of misuse and a ceiling effect that limits the potential for overdose.
- Teenagers using Suboxone should be closely monitored to ensure proper dosage and to address any emerging signs of misuse or diversion.
Contact us at (845) 479-6888 for more information on our specialized teen drug recovery assistance programs.
Brief History of Suboxone
Suboxone, a prescription medication to treat opioid addiction, has a relatively brief but impactful history. Approved by the U.S. Food and Drug Administration in 2002, it marked a significant advancement in addiction treatment.
Comprising buprenorphine and naloxone, Suboxone helps curb cravings and withdrawal symptoms associated with opioid dependence. Its introduction was a response to the growing opioid epidemic, providing a safer alternative to methadone.
Over the years, Suboxone has become a cornerstone in medication-assisted treatment programs, offering a balance between effectiveness and reduced risk of misuse. However, debates surround its accessibility, with concerns about diversion and misuse.
Despite the controversies, Suboxone continues to play a pivotal role in addressing opioid addiction, fostering hope for recovery and improved quality of life for those grappling with substance use disorders.
Understanding Suboxone’s Ingredients
Suboxone is a prescription medication used in the treatment of opioid addiction. It contains two main active ingredients: buprenorphine and naloxone.
Let’s take a closer look at each of these components:
Buprenorphine: Buprenorphine, a partial opioid agonist, is a key component of Suboxone. It interacts with the same brain receptors as opioids, albeit to a lesser extent. Its primary function is to diminish cravings and alleviate withdrawal symptoms associated with opioid dependence.
A notable characteristic of buprenorphine is its extended half-life, allowing for less frequent dosing compared to other medicines used in opioid addiction treatment.
Naloxone: Naloxone, an opioid antagonist, complements buprenorphine in Suboxone. As an antagonist, it blocks the effects of opioids. In Suboxone, naloxone serves as a deterrent to misuse. When taken orally as prescribed, naloxone has minimal absorption into the bloodstream.
However, if Suboxone is improperly used by injecting or snorting, the naloxone becomes active, inducing withdrawal symptoms in those dependent on opioids. This mechanism discourages inappropriate use of the medication.
Medical Uses for Suboxone
Suboxone is commonly prescribed in the treatment of opioid dependence, specifically for opioid addiction.
Here are some medical uses for Suboxone:
Suboxone in Opioid Addiction Treatment: Suboxone, comprising buprenorphine and naloxone, is a cornerstone in treating opioid addiction. Buprenorphine, a partial opioid agonist, effectively manages cravings and withdrawal symptoms, facilitating a smoother path to recovery for individuals grappling with opioid dependence.
Pain Management Alternative: Beyond addiction treatment, Suboxone demonstrates effectiveness in pain management. Particularly in cases of chronic pain, where conventional opioids might carry a risk of abuse or dependency, Suboxone provides a balance.
It offers pain relief while mitigating the euphoric effects associated with full opioid agonists.
Addressing Neonatal Abstinence Syndrome (NAS): Suboxone plays a crucial role in reducing withdrawal symptoms in newborns born to mothers with opioid dependency. By addressing Neonatal Abstinence Syndrome (NAS), Suboxone helps improve the well-being of infants facing challenges associated with maternal opioid use during pregnancy.
Minimizing Misuse and Diversion: The inclusion of naloxone, an opioid antagonist, in Suboxone’s formulation enhances its safety profile by minimizing the potential for misuse and diversion. This aspect distinguishes Suboxone from other opioid medications, contributing to its role as a responsible and effective therapeutic option.
Evolving Applications in Research: Ongoing research continues to unveil the versatile applications of Suboxone, emphasizing its potential as a valuable tool in addressing various aspects of opioid-related health challenges.
As insights grow, Suboxone’s multifaceted role in both addiction treatment and pain management solidifies its position as a promising solution within the medical field.
Suboxone and the Human Brain
Suboxone’s effects on the brain are complex. By activating opioid receptors to a lesser extent than full agonists, buprenorphine provides a milder, more stable effect. This can help individuals function without the intense highs and lows associated with opioid use.
The inclusion of naloxone in Suboxone is crucial in preventing misuse. If injected, naloxone can rapidly reverse the effects of opioids, leading to severe withdrawal symptoms. This discourages individuals from using Suboxone in a way other than prescribed.
Misconceptions About Suboxone
Addressing common misconceptions is crucial:
- Suboxone Substitutes One Addiction for Another
Reality: Suboxone, part of medication-assisted treatment (MAT), helps manage withdrawal and cravings under medical supervision, promoting controlled reduction of opioid dependence.
- Suboxone Is Only for Short-Term Use
Reality: Suboxone is a long-term maintenance treatment, with duration varying per individual. Some benefit from extended use to sustain recovery and prevent relapse.
- Suboxone Is A “Magic Cure” For Addiction
Reality: While effective, Suboxone complements a comprehensive approach involving counseling, therapy, and lifestyle changes. It addresses symptoms but not the root causes of addiction.
- Suboxone Is Easily Abused
Reality: With a lower abuse potential than full opioids, naloxone in Suboxone deters misuse by injection. When taken as prescribed, under supervision, abuse risks significantly decrease.
- People On Suboxone Are Not Truly in Recovery
Reality: Medication-assisted treatment, including Suboxone, is recognized as a valid form of recovery. It stabilizes lives, reduces relapse risk, and enhances engagement in counseling and therapy.
- Suboxone Is Only for Severe Cases of Opioid Addiction
Reality: Suboxone is prescribed across a spectrum of opioid use disorders, from moderate to severe. Individual assessments guide its use based on addiction history, medical conditions, and treatment needs.
By dispelling these misconceptions, a more accurate understanding of Suboxone’s role in comprehensive addiction treatment can be promoted, encouraging individuals to seek effective support tailored to their specific needs.
Potential for Abuse
Despite its benefits in treating opioid addiction, Suboxone does carry a potential for abuse. As a partial opioid agonist, it binds to the same receptors in the brain as opioids, albeit with less intensity. While this minimizes withdrawal symptoms and cravings, it also opens the door for individuals to misuse the medication, seeking the euphoric effects associated with stronger opioids.
The naloxone component is intended to deter abuse by inducing withdrawal symptoms if Suboxone is injected, but it may not eliminate the risk. Close monitoring by healthcare providers and adherence to prescribed doses are crucial to prevent misuse.
A comprehensive treatment plan that includes counseling and behavioral therapy is essential to address the underlying causes of addiction, reducing the likelihood of Suboxone abuse and supporting lasting recovery.
Frequently Asked Questions (FAQ)
What happens when you first start taking Suboxone?
Suboxone, a medication for opioid dependence, contains buprenorphine and naloxone. When initially taken, it alleviates withdrawal symptoms and cravings, attaching to opioid receptors.
However, if opioids are still present, naloxone counters their effects to deter misuse. It’s crucial to follow prescribed guidelines by doctors for a safe and effective transition to recovery.
Why does Suboxone block opiates?
Suboxone contains buprenorphine, a partial agonist. It blocks the effects of other opioids, like heroin, because it binds to the same receptors in the brain. This binding prevents stronger opioids from having their usual effects, helping patients overcome opioid misuse.
The naloxone component further deters opioid effects.
How does buprenorphine work in the brain?
Buprenorphine, found in Suboxone, works as a partial agonist in the brain. Unlike full agonists, which activate receptors strongly, buprenorphine has a milder effect. This helps reduce opioid withdrawal symptoms and cravings, making it a crucial component in treating opioid addiction as part of a comprehensive healthcare plan.
Help Your Teen With Suboxone Recovery
Our dedicated teen treatment center is committed to guiding teenagers toward a life of recovery and resilience.
Experience the power of our residential treatment program, meticulously designed to nurture young minds through a unique fusion of art and music therapy, educational workshops, and invigorating recreational activities.
Moreover, our skilled therapists work tirelessly to empower young adults, fostering healthy coping mechanisms that pave the way for a brighter tomorrow.Your teen deserves a future filled with joy and health. Contact us at (845) 479-6888 today.